Quitting smoking during a pandemic
In OTC
Follow this topic
Bookmark
Record learning outcomes
More people than ever could be seeking to quit smoking given the higher risks smokers are known to face with Covid-19. Yet the pandemic is also creating additional challenges for those wanting to quit

Key facts
• The proportion of smokers quitting in the past year is 8.5 per cent – almost twice the 4.3 per cent rate in 2019
• During the Covid-19 pandemic a noticeable development has been the introduction of the #quitforcovid campaign
• Pharmacy teams should be knowledge-able about vaping and smoking cessation so they can answer any questions
It has been estimated that 1 million people quit smoking in the UK during the first wave of the coronavirus pandemic1 but many, unfortunately, will relapse. Mixed messages around nicotine and Covid-19 could be having an effect on motivation, while loneliness, sadly all too common in lockdown, has been shown to cause more people to fail in their quit attempts. Stress around job security and financial worries is also hindering smokers making a successful quit attempt.
While it is encouraging that so many people tried to quit smoking, research has also shown that the first national lockdown led to an increase in second-hand smoke exposure for children as families were confined to their homes.
Most community pharmacies in England are now classed as healthy living pharmacies under the national contractual framework and there are many trained health champions who offer smoking cessation interventions. Unfortunately, over the years there has been a downward trend in community pharmacies offering more intense behavioural support alongside effective pharmacotherapy treatments.
In 2014/15, around 19 per cent of all quit attempts in the English NHS smoking cessation service were made through community pharmacies (84,961 of 450,582)2. However, between April-December 2019, that had fallen to around 16 per cent (25,315 of 155,645).3
The new contractual framework sets out how important the role of community pharmacy is in supporting the NHS Long Term Plan. One of the suggested ideas is the introduction of stop smoking support for those beginning a programme of smoking cessation in secondary care and referred for completion in community pharmacy. Indeed, this service is due to launch in the new year.
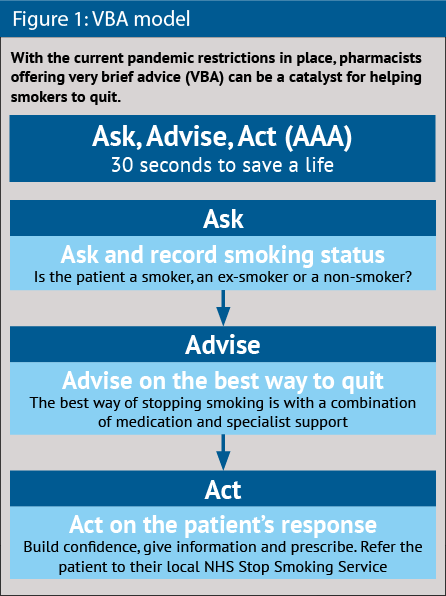
This may be one way of reviving pharmacy’s smoking cessation role but it is not enough to only treat sick patients referred from hospital who are tobacco dependent. Every contact needs to count and it has never been more important to offer very brief advice to smokers seeking to quit (see Figure 1).
Stopping smoking reduces the risk of developing many fatal diseases and delivers immediate benefits – for example, improved blood pressure, and reduced respiratory infections and heart disease.
Current smokers are five times as likely to get influenza and twice as likely to get pneumonia as non-smokers – major factors in the winter pressures faced by the NHS, which could be so much worse this year due to the Covid pandemic.
Varenicline in combination with NHS support has consistently been shown to be the most effective combination
Has the pandemic actually led to more smoking?
UCL’s Smoking Toolkit Study shows an increase in quitting success rates this year, but new research shows that is just one side of the story. Data gathered by Smoke Free, an app that supports smokers through quitting, shows that:
• 10 per cent of people in the UK have started or re-started smoking as a direct result of the pandemic
• A further 10 per cent were going to quit but decided not to once Covid-19 hit
• A third of smokers admitted to smoking through the pandemic, despite knowing it is likely to make them more susceptible to serious complications should they contract Covid-19
• Another 10 per cent said that working from home during lockdown has enabled them to smoke more than when they were going to their usual place of work.
Sixteen per cent of smokers said they would go to the pharmacy as their first port of call for stop smoking advice, 30 per cent would visit the GP and 15 per cent would seek advice from the internet. Of the smokers who had tried to quit before, 40 per cent had done it on their own, while only 18 per cent had used NHS services.
“There is good evidence that Covid-19 is motivating some people to quit, but the data we’ve gathered indicates that it is also having the opposite effect on others,” says behavioural scientist and founder of the Smoke Free app, Dr David Crane. “For them, Covid-19 has actually increased their desire to smoke.
“This might seem counterintuitive at first: why would people want to start smoking now of all times? It is possibly because now is a very unsettling and upsetting time for many people, so it is understandable that some want to seek out things that bring pleasure. For smokers, that’s smoking.”
The Smoke Free app has been downloaded 5 million times.
Licensed treatments
There are currently many effective licensed treatments available to help smokers quit (e.g. varenicline, bupropion and nicotine replacement therapies). NHS evidence-based support alongside these treatments can improve a person’s chances of stopping smoking by at least three-fold.
For appropriate patients varenicline in combination with NHS support has consistently been shown to be the most effective combination. The good news is that many varenicline PGD services are being set up across the country, making it more easily accessible to the patients who need it the most.
Remote consultations
Many clinicians are now offering behavioural support via remote consultations due to Covid but many considerations need to be factored in for telephone and video consultations that differ from those for face-to-face services.4 Current evidence suggests that more frequent telephone follow-ups (similar to the six-week face-to-face sessions) will improve a person’s chances of cessation.5
The added advantage that video consultations may bring over telephone follow-ups is that they are more personable, which may aid the rapport- building process and provide an opportunity for patients to demonstrate understanding.
When it becomes safe to do so again, face-to-face consultations should be carried out for people where needed, as not everyone will have access to technology, or it may not suit them – for example if they have hearing difficulties, language barriers or mental health challenges.
Carbon monoxide monitoring has had to be paused, which is unfortunate as not only does it help verify smoking status, but people who go smoke-free find the readings motivational. It should be noted that shisha/water pipe smoking is on the rise and there needs to be greater awareness about how sharing the mouthpiece increases the risk of spreading Covid-19.
Apps and web-based support
During the pandemic a noticeable development has been the #quitforcovid campaign alongside the many support apps that are now available. One example is the NHS Smokefree app, which follows NICE guidance, incorporates most of the behaviour change techniques used in face-to-face services and has evidence of effectiveness from two randomised control trials.6 Artificial intelligence is also being explored by some NHS services (e.g. Quit with Bella and its ‘Robo-Coach’).7
Apps can complement existing NHS support services or can be offered to people looking to stop cold turkey or using pharmacotherapy alone.
The effects of Covid-19 are going to continue for a long time. As and when the NHS resumes routine quit services, understanding where digital technology can help and add most value will be more important than ever for pharmacists.
The added advantage that video consultations bring over telephone follow-ups is that they are more personable
Quit support via an app
With over 40 years of experience in NRT innovation, Nicorette uses a three-pronged approach to support quitters with behavioural scientists and leaders in health tech to:
• Help smokers build awareness and knowledge of their smoking behaviour
• Provide confidence and motivation to quit
• Equip smokers with coping and relapse prevention skills.
This year Nicorette launched the first connected stop smoking product that brings together NRT and a tailored level of support for each smoker’s individual quit journey.
Over two years of research went into the development of Nicorette QuickMist SmartTrack, while a U&A study was carried out across seven markets to ensure it supported quitters’ needs.
Nicorette QuickMist SmartTrack links its nicotine mouth spray with a behavioural support app that allows patients to:
• Track their NRT product usage with a simple tap to their smartphone
• Set a personal quit plan, track progress towards their quitting goals and receive motivational tips to help them stay on track.
E-cigarettes and vaping
Pharmacy teams should be knowledgeable about vaping so they can answer any questions and be able to direct people to the most up-to-date sources of information.
Some pharmacies will sell vapes to support people to stop smoking or reduce the amount of tobacco consumed. However, as there are so many different vapes on the market, finding the right device, flavour and nicotine strength that suits an individual will require more extensive training and stocking a broader range of products. Another option is to build a relationship with a reputable vape shop. If there is a local specialist service, they can also advise on the best steps to take.
Vaping can be a useful aid to stopping smoking and recent Cochrane data has shown it to be more effective than even gum or patches. If six people in 100 quit by using NRT, 10 people in 100 would quit by using vapes containing nicotine. This means an additional four people in 100 could potentially quit smoking with nicotine-containing vapes.
It may not sound like a lot, but there are nearly 3.2 million people currently using vapes, making it by far the most popular stop smoking aid. For every two people pharmacists can help abstain from smoking, one premature death will be avoided.8
According to NICE, vapes are substantially less harmful to health than smoking but are not risk-free. Evidence about vapes is still developing, including that on their long-term health impact. Bearing the risk in mind, the Primary Care Respiratory Society (PCRS) suggests that patients should be offered the most effective and least harmful methods to support a quit attempt – currently varenicline or a combination of two NRT products (usually long and short acting) with evidence-based support.
As there aren’t many trials assessing long-term safety, all individuals using vapes to support a quit attempt should be supported in cutting down their level of nicotine at a rate that still enables them to abstain from smoking tobacco with a view to ultimately stopping nicotine as well. This should not be done at the expense of relapsing to smoking and patients should be supported in longer-term NRT if they choose that option. Although vapes are not licensed medicines, they are regulated by the Tobacco and Related Products Regulations 2016 and those that are legally sold in the UK will be registered with the MHRA. Pharmacists should report any adverse reactions in the usual way.
So what advice should pharmacy teams provide to people concerned about vaping?
- For people who do not smoke or have never smoked, the advice is to not start vaping
- Do not sell vapes to anyone under the age of 18 years and advise users to keep them out of the sight and reach of children and pets
- If smokers are not keen on licensed treatments, then switching completely to vapes is significantly less harmful than continuing to smoke and should be encouraged
- It is currently unknown what effect vaping may have on susceptibility to severe disease if the user gets Covid-19
- For most people vaping remains significantly less harmful than smoking and it is very important that they avoid returning to smoking.
In conclusion, the pandemic means these are challenging times for smokers who want to quit. But it provides a timely opportunity, too. Pharmacists should look to step up their support for would-be quitters, now more than ever.

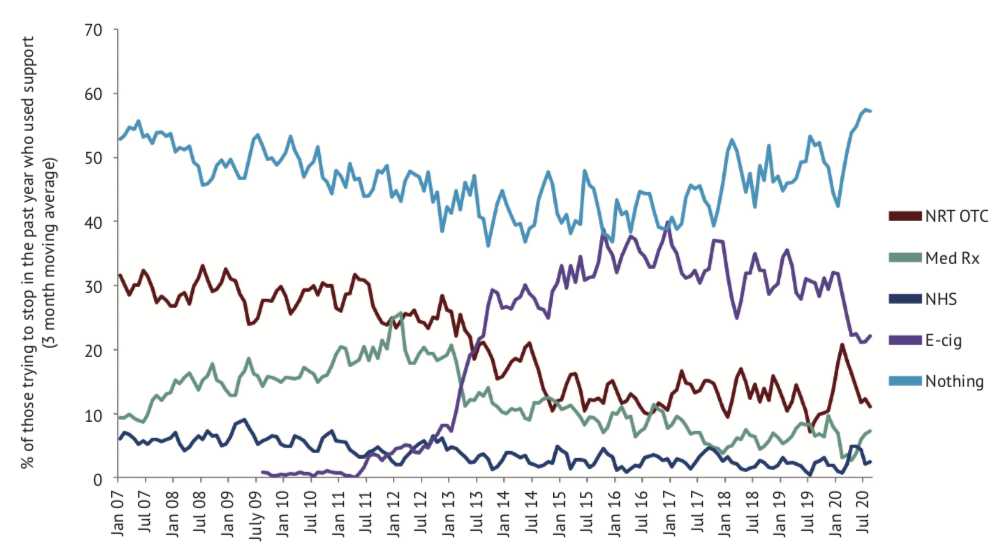
How are smokers trying to quit during the Covid-19 pandemic?
Since January 2020 there has been a clear upward trend in people trying to stop smoking with no support or no treatment (approximately 50 per cent). Unfortunately, this is the least effective way of stopping, with data showing only around 2-3 per cent of people will have been successful after one year.
However, this may be different during a pandemic, and NHS and PHE data may provide some better insight later in the year.9
Since 2014, e-cigarettes/vaping have been a popular method for helping people stop, but in recent months there has been a steady decline in use (approximately 25 per cent). While there has been a rise in over-the-counter NRT (approximately 15 per cent), some data has shown this method to be not very effective – possibly because people may not be using the treatment properly (e.g. poor technique, under-dosing, terminating usage too soon).
NHS support and prescribed therapies have stayed steady but not been maximised (<10 per cent), which is unfortunate as these methods have the strongest evidence base of efficacy and safety.
References
- Action on smoking
- The NHS Information Centre, Lifestyles Statistics. Statistics on NHS Stop Smoking Services in England, April 2014 to March 2015 Final report. The Health and Social Care Information Centre; 2015.
- NHS Digital
- NCST
- Cochrane
- NSCT: Remoste consultations
- Quit with Bella
- NCBI
- NHS Digital.
